Since the onset of the coronavirus pandemic in March, Delta Ambulance trucks have been navigating central Maine, the virus a constant concern on every call that has dictated the way paramedics and emergency medical technicians approach their work and their patients. Wearing a mask and developing the ability to assess a patient’s symptoms from 6 feet away have become part of the mosaic of ritual routines such as washing hands.
While Maine enjoyed low case numbers and few deaths during the dry, warm summer where space facilitated distancing, the colder, wetter fall has driven people inside. Schools have started up again and the case numbers and deaths have risen. A major source of stress now confronts emergency medical services providers: staffing.
“Staffing is huge, because if you’re short staffed that means everyone else has to pick up the slack,” Delta purchasing manager Phil Smith said recently. “Staffing is of higher concern than PPE at this point.”
In March, first responders, medical personnel and hospitals were scrambling for personal protective equipment regardless of the cost. Now Delta is set up for six months to a year for PPE.
“To put it into perspective, when this started back in March, I spent up to a dollar per surgical mask. Now I’m paying 7 cents,” Smith said. “Unfortunately you can’t order staff.”
In much the same way there was a scramble for PPE, there is an ongoing scramble for licensed field providers to fill the ambulances. Retention rates are low because of several factors, including low wages for intense work. There have been delays in licensing new EMS staff because the pandemic forced closures of schools and hospitals delayed clinical hands-on training.
“It’s constant recruitment looking for individuals to come and work for you,” said Tim Beals, executive director of Delta Ambulance. “I don’t want to call it a revolving door. You’re recruiting in the state and out of the state. And oftentimes, all EMS services and all fire departments, we’re all in this … It’s like we’re recruiting from each other.”

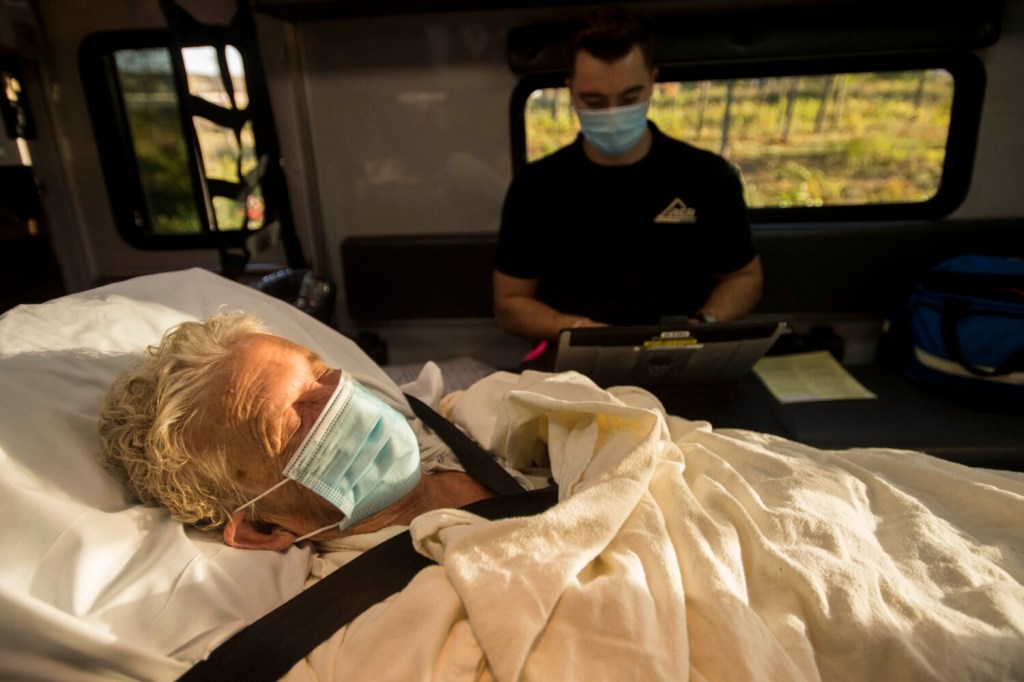
Corie McCarthy, a paramedic with Delta Ambulance, treats a patient Tuesday during a transfer from Inland Hospital to Eastern Maine Medical Center in Bangor. Michael G. Seamans/Morning Sentinel
TOUGH WORKING CONDITIONS
The long, drawn out duration of the pandemic has been a challenge for EMS programs that license new providers and for EMS field providers who are working long hours because of understaffing.
Describing the conditions EMS providers are working through, Rick Petrie, executive director of Atlantic Partners EMS, a resource agency for EMS in 12 of Maine’s 16 counties, said, “This is like a big mass casualty incident, but it involves the entire state of Maine. And not only that, the only good news about a mass casualty, it’s over in a couple of hours. That’s the only good that ever comes from that. It’s over in a couple of hours. This may not be over in a year.”
Rural services have lost retirees who act as volunteer ambulance drivers because they couldn’t risk exposure, Petrie said, and rural fire chiefs and other EMS members fear bringing the disease home to their families. “It’s taking a toll on people,” he said.
The lack of staff has a ripple effect throughout the healthcare continuum, according to Petrie. “Even without COVID, EMS in Maine, we need help. We’re struggling for personnel … and coupled with that our hospitals are in trouble in the state and are struggling to figure out how they are going to operate. And EMS is part of that equation. We move their patients. We assist in their communities, and so we need to look for other alternatives as well.”
Delta’s director, Beals, believes it takes a special person to take on the responsibility of being one of the first at the scene of a disaster, however big or small the numbers involved.
“It’s a noble profession,” Beals said. “The responsibilities we’re given. You get the opportunity to make a difference in someone’s life, and that’s pretty unique. “

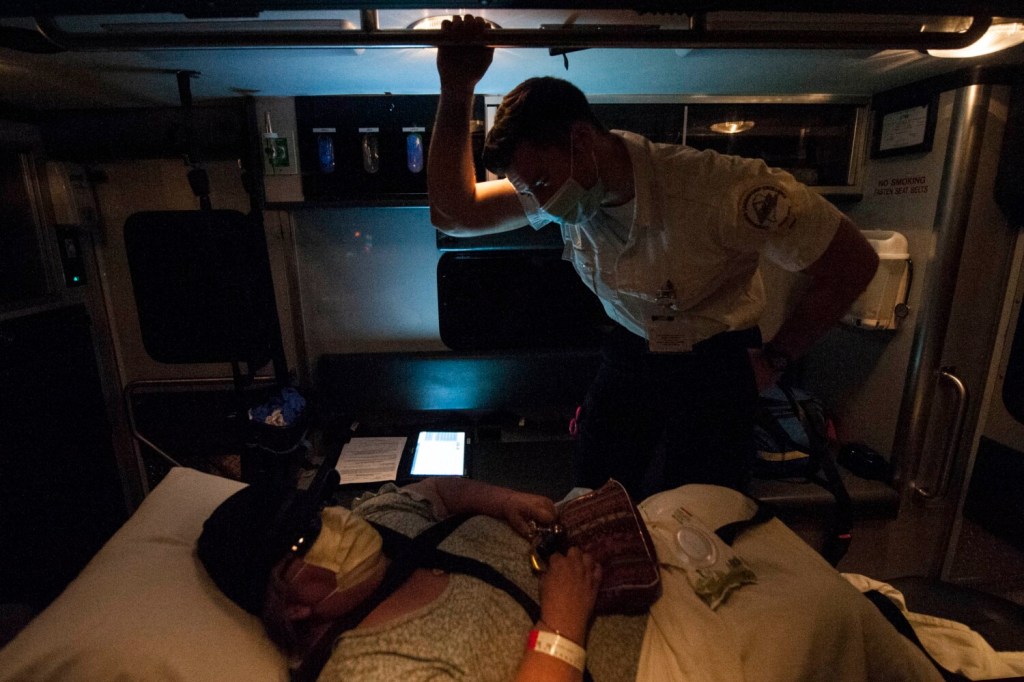
Rebecca Quinn, a paramedic with Delta Ambulance, assesses a patient as she looks for a spot to place an IV during a July 11 call that warranted personal protective equipment to protect against possible COVID-19 exposure. Michael G. Seamans/Morning Sentinel
Beals exemplifies what you might expect from a lifer in the EMS industry. His story began in 1977 in southern Vermont where he cut his teeth as a volunteer on the Guilford fire department. From there he went to the University of Vermont and received a degree in secondary education in 1977. Unable to find a teaching job, Beals entered paramedic school and made it a career.
But as Delta paramedic Rebecca Quinn said, “You can make it a career, but you’re not going to get paid as much. There’s nowhere to promote.” And then there is the stress, the hours and now the coronavirus.
THE DISEASE THAT SABOTAGES TRAINING
COVID restrictions, school shutdowns, remote learning and positive tests among instructors and students have clogged the education and licensing of new EMS providers.
Kirk Burrows, 25, an EMT with Delta for the past three years, has been working toward his paramedic certification since September 2019. He is in a 14-month paramedicine class run by United Training in Lewiston. Fulfilling the hands-on learning required to do the job has become a major hurdle.
“It was a nightmare,” Burrows said. “April 1st was when we went to all online, and all of our clinicals were canceled. And we were like that until August. August was when we could meet back up in person again for normal classroom time. And our clinicals only got cleared to restart at the end of October. So we essentially scrapped about half of our clinical requirements so that we could actually meet them. So we did away with a lot of the hospital time and a lot of the field time.”
Exposure to coronavirus itself has also stymied training. The EMS instructors all work at services in the field, and any student beyond the Basic EMT level of training is likely employed by a service. Exposure potential is high and can disrupt class schedules. Exposure of anyone in class can mean several providers have to be quarantined and are out of service, further stressing the fragile staffing numbers.

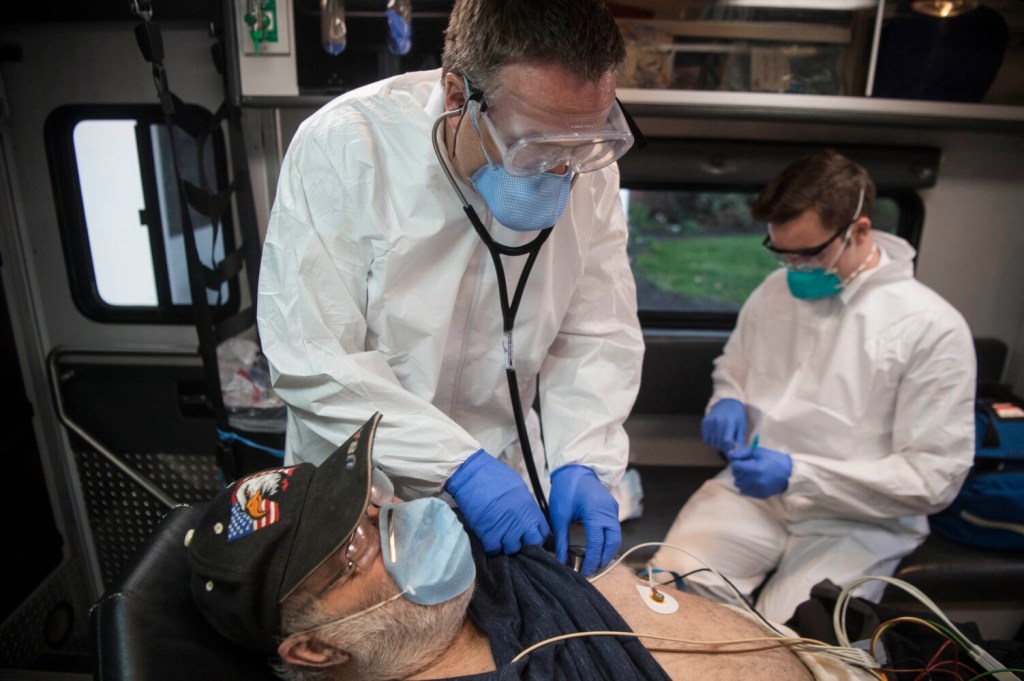
Rebecca Quinn, paramedic, right, fills out her charts as her partner Nathaniel Lombardi, an advanced EMT, center, trains a new hire, basic EMT Chris Wildes at Delta Ambulance in Waterville on Aug. 23. Lombardi, the field training officer, instructs Wildes on how to use the child restraint system. Michael G. Seamans/Morning Sentinel
“I got exposed three times last month,” Burrows said. “So I missed an extra two weeks of class on top of what we had already missed in person, and I missed more clinicals. And other people are in similar boats. But we managed to finish with going only one week over.”
Other people in the class have been exposed and tested positive, forcing other two-week shutdowns, but Burrows said, “We test per exposure. So it’s not like you get one every two weeks or something.”
Burrows is persistent. His mother works as an EMT and was one of the first to respond to the World Trade Center on 9/11 to sift through rubble looking for survivors and bodies. His father is a career firefighter who asked him to take a meandering path to the EMS life. “I went from garbage man to retail associate to factory worker to dishwasher to future paramedic … all by my bootstraps.”
A PROBLEM IN NEED OF SOLUTIONS
Petrie of Atlantic Partners EMS said organizations are paying a significant amount of overtime and relying on mutual aid to answer calls, which puts a strain on other communities and services. “It’s this massive shell game that we’re trying to just keep the system floating and keep people responding when somebody needs help.”
Changes have been made to the educational system. Petrie’s organization works with Kennebec Valley Community College and Eastern Maine Community College. Besides online learning, protocols to avoid exposure and transmission during in-person sessions have been instituted, and a new assessment program using virtual reality goggles has been reviewed.
But the risk of exposure is still a worry and the positivity rate is rising, Petrie said. Delays are endemic.

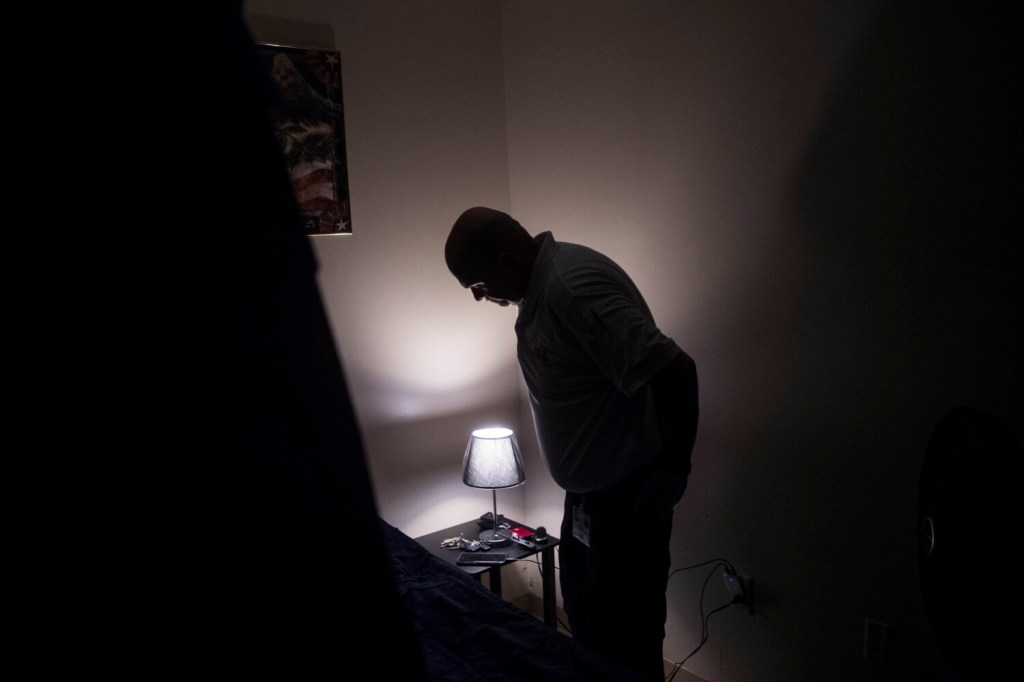
Nathaniel Lombardi, an advanced EMT with Delta Ambulance, and his partner, paramedic Rebecca Quinn, remove a patient from an assisted living facility May 21 as family reflected in the ambulance window watch from a distance. Michael G. Seamans/Morning Sentinel
“KVCC was supposed to graduate in December this year and start again in January, and they have delayed the start of their program until next September,” Petrie said.
Staffing problems existed before the onset of the pandemic; COVID has made the problems worse, Petrie said, adding that a short-term and a long-term solution to the problem is needed “or else we are going to start to feel significant effects on the EMS system in the state, that you start to see increased response times and fewer people.”
Rebecca Quinn was looking for a service that paid better and wanted to be close to family when she came to New England. Originally from Connecticut, Quinn moved from Marion County Fire Rescue in Florida. She worked as a paramedic for four years before moving to work for Delta Ambulance where she has been for the last two years.
“This whole industry, everywhere else I’ve worked, is short staffed. It’s normal for me. It doesn’t affect me as much as some others.”
Quinn is applying to graduate school for a master’s in public health.
Send questions/comments to the editors.



























Comments are no longer available on this story